- Home
- Symptoms Directory
- Colitis symptoms
Colitis symptoms: What are the early signs of colitis?

Overview: What does colitis feel like?
Colitis is swelling of the inside lining of the colon. The inflammation can be the result of infections, autoimmune reactions, toxins, drugs, decreased blood flow, radiation therapy, or other problems. No matter what the cause, most people will experience colitis as watery diarrhea. Sometimes it will have blood, but not always. Abdominal pain and cramping are typical. Most people will also experience an urgent need to pass stools. Sometimes, that urgent need to defecate won’t go away even when the large intestine is emptied. Fever and fatigue are also possible, but it depends on the cause. Most of these symptoms have treatments, but in most cases, healthcare providers will target the cause for treatment.
Key takeaways:
Colitis is a common health condition that can affect anyone regardless of age, sex, race, or ethnicity.
Early signs of colitis include watery diarrhea and abdominal pain.
Serious symptoms of colitis such as persistent watery diarrhea, severe abdominal pain, blood in the stools, or worsening of symptoms, may require immediate medical attention.
Colitis is caused by infections, autoimmune responses, decreased blood flow to the colon tissues, and other problems. Risk factors for developing colitis symptoms include if you are white, of Jewish ethnicity, increasing age, undergoing abdominal radiation treatment, taking antibiotics, consuming contaminated water or food, or have food allergies, sickle cell anemia, a family member with inflammatory bowel disease, or a weakened immune system.
Colitis requires a medical diagnosis.
Symptoms of colitis generally do require treatment. They typically resolve but recovery time depends on the cause.
Treatment of colitis will vary depending on the cause and may include antibiotics, antiparasitic medications, antiviral medications, anti-inflammatory medications, immune suppressants, fluid replacement, anti-diarrheal medications, and, in some cases, surgery.
Untreated colitis could result in complications like dehydration, intestinal perforation, intestinal obstruction, abscess, fistulas, incontinence, colon cancer, and complications due to certain bacterial infections.
Use coupons for colitis treatments like mesalamine, balsalazide, and Dipentum to save up to 80%.
What are the early signs of colitis?
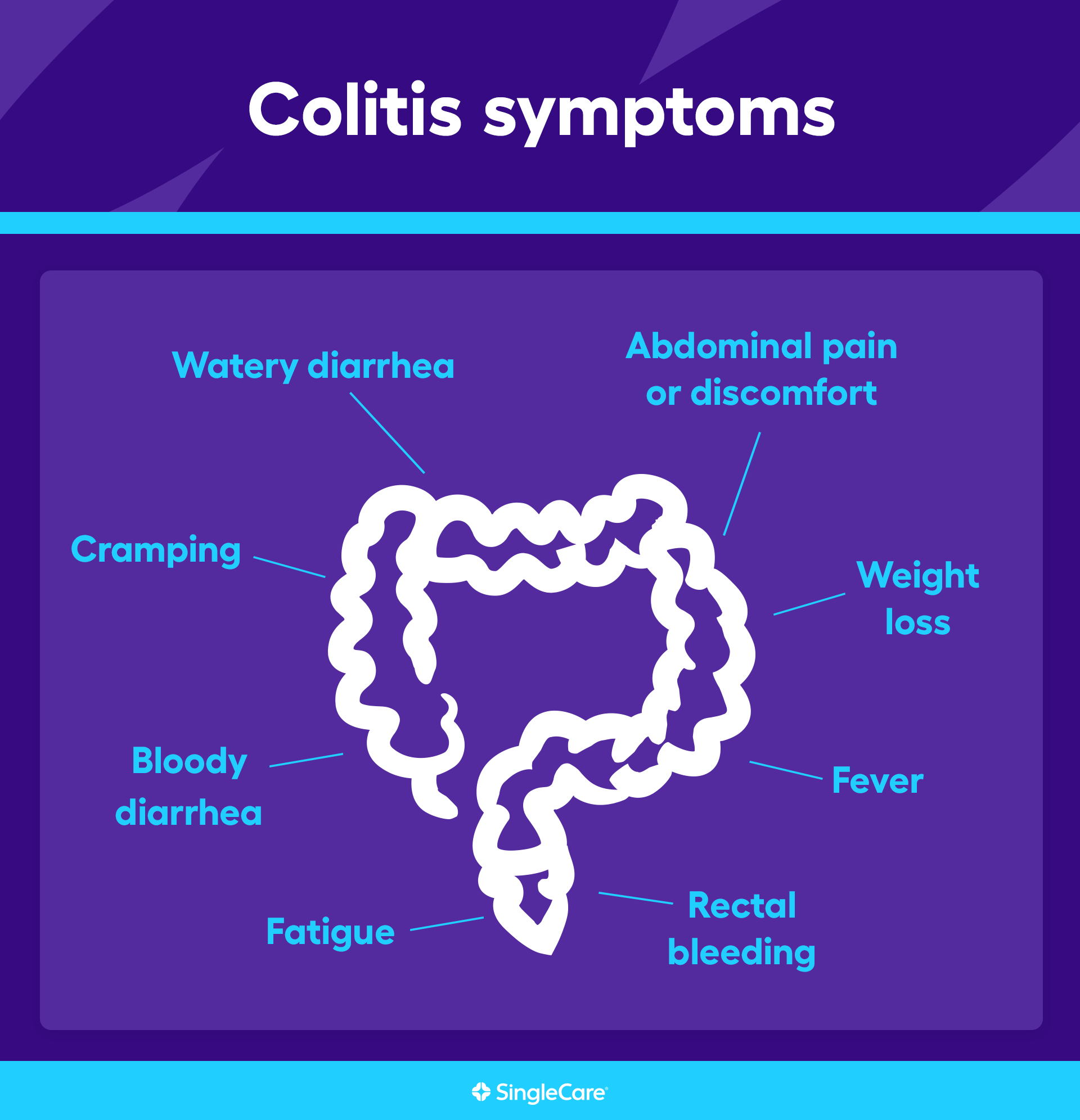
The early signs of colitis typically are:
Watery diarrhea
Abdominal pain or discomfort
Cramping
Other colitis symptoms
While colitis is marked by watery diarrhea, other symptoms are possible, as well. Some may be related to the swelling, but others may be secondary. The symptoms of colitis include:
Watery diarrhea
Abdominal pain or discomfort
Abdominal cramps
Bloody diarrhea
Fever
Bowel movement urgency, sometimes when the colon is empty
Rectal bleeding
Fatigue
Loss of appetite
Weight loss
Depending on the cause, secondary symptoms might include:
Joint pain
Arthritis
Eye swelling
Swelling in the mouth
Mouth sores
Colitis vs. Crohn’s
Colitis has many causes. One possible cause is the immune system. In this case, the body’s immune system attacks healthy colon tissues. Called ulcerative colitis, this type of colitis is grouped with Crohn’s disease as inflammatory bowel disease (IBD). Inflammation due to ulcerative colitis is limited to the large intestine and rectum. On the other hand, Crohn’s disease can affect the entire gastrointestinal system, usually the small intestine. However, the colon can be affected, too. The symptoms are largely identical. Although ulcerative colitis is limited to the colon, the inflammatory response can cause problems throughout the body, so the body-wide symptoms of ulcerative colitis are similar to symptoms of Crohn’s. That’s not true of other types of colitis.
| Colitis | Crohn’s | |
| Shared symptoms |
|
|
| Unique symptoms |
|
|
RELATED: Ulcerative colitis vs. Crohn’s: Compare causes, symptoms, & treatments
Types of colitis: How can I tell which one I have?
Healthcare professionals distinguish between the various types of colitis based on the cause. After all, colitis treatment will be targeted at the cause. Because all types of colitis cause diarrhea and have similar symptoms, it’s hard to tell which type of colitis a person has until a healthcare provider has performed blood tests, stool tests, and examined the colon lining.
The types of colitis are:
Infectious colitis: inflammation of the colon caused by a bacterial, parasitic, or viral infection
Ulcerative colitis and ulcerative proctitis: inflammation of the lining of the colon or rectum caused by an immune system attack on the tissues lining the colon
Ischemic colitis: colon inflammation resulting from reduced or obstructed blood flow to a part of the colon often as a result of a blood clot—common symptoms are extreme abdominal pain and bloody stools
Allergic colitis (or eosinophilic colitis): most commonly seen in newborns and infants, allergic colitis is caused by white blood cells invading the colon tissues in response to a food allergy such as a milk protein allergy
Microscopic colitis: inflammation of the colon due to several unrelated causes including drugs, smoking, bacteria, viruses, or autoimmune disorders—the distinguishing feature is chronic, daily diarrhea
Radiation treatment to the abdomen can also cause colitis, but it also usually involves the small intestines. The radiation injures the intestines, resulting in inflammation and diarrhea. The condition is usually temporary, but some people will have chronic or even lifelong intestinal problems after radiation therapy.
When to see a doctor for colitis symptoms
See a doctor if you experience any of these symptoms:
Watery diarrhea persists for two days or more
Blood is present in diarrhea
Abdominal pain is severe or gets worse
Abdominal pain isolated to the left side or right side of the abdomen
Fever gets very high
Dehydration starts causing symptoms like thirst, decreased urination, dark urine, weakness, and lightheadedness
To make a diagnosis, a healthcare professional, physician, or specialist in the digestive system will need to perform a physical examination and take a thorough history. Blood tests and stool tests will be used to identify the cause. An X-ray may be used, but a CT scan is more useful in identifying where the problem is located.
To make a definitive diagnosis, a doctor or gastroenterologist will need to examine the lining of the colon and rectum using an endoscope, a camera attached to a flexible tube. To examine the colon, they will either examine the rectum, anus, and colon above the anus with a short endoscope (flexible sigmoidoscopy) or the entire colon with a longer endoscope (colonoscopy). In some cases, the doctor may need to examine other parts of the digestive tract such as the esophagus or small intestine. Depending on the suspected cause, the doctor may perform a biopsy by removing tissue samples from the colon for microscopic analysis.
Complications of colitis
Complications of untreated colitis will vary depending on the cause. Possible complications include:
Dehydration
Abscess
Intestinal tears or holes
Intestinal obstruction
Incontinence
Colon leakage
Colorectal cancer
Severe complications of bacterial infection, including body-wide nerve damage, kidney damage, brain disease, seizures, and extreme and life-threatening inflammation of the colon (toxic megacolon)
How to treat colitis symptoms
Not all cases of colitis will require treatment, but some types of colitis do require treatment. For the most part, treatment options will focus on the underlying cause. Sometimes medications may be used to reduce inflammation or control diarrhea.
Treatment usually consists of:
Antibiotics to treat or prevent bacterial infection
Antiparasitic drugs to eliminate parasite infections
Antiviral drugs to control some types of virus infections
Aminosalicylates (5-ASA), immune-modulating drugs, corticosteroids, or biologics to control inflammation due to ulcerative colitis
Corticosteroids (budesonide), antidiarrheal drugs, or immune-modulating drugs to induce remission in people with microscopic colitis
Surgical removal of part of the colon in extreme cases of ischemic colitis, inflammatory bowel disease, radiation enteritis
Lifestyle and dietary changes in people with ulcerative, allergic, or microscopic colitis
In some people, over-the-counter medications might help such as antidiarrheal drugs and pain relievers. However, get medical advice from a healthcare professional before using these drugs.
Living with colitis
Many people who experience a bout with colitis will get over it. Other people, though, may have chronic colitis conditions such as inflammatory bowel disease or microscopic colitis. For them, living with colitis means preventing flare-ups, effectively managing those flare-ups, and maintaining quality of life. Here are some tips:
Take all medications as instructed
Keep a symptom and drug side effects diary to help spot triggers and share with healthcare providers
Follow all dietary recommendations
Maintain general health through regular physical checkups, dentist visits, and vaccinations
Avoid unhealthy habits such as smoking and drinking
Manage stress
Avoid certain foods like dairy products
Most importantly, see a doctor if you experience certain symptoms
A short bout with diarrhea and a bit of stomach pain is usually no cause for concern. However, bloody diarrhea, severe abdominal pain, or watery diarrhea that just doesn’t get better could be cause for worry. The problem could deteriorate. The only way to be sure is to see a doctor who can figure out the cause and the appropriate treatment.
FAQs about colitis symptoms
What are the three most common types of colitis?
Colitis is distinguished by the underlying cause. Infectious colitis is due to a colon infection. Ulcerative colitis is caused by an autoimmune attack on the colon. Ischemic colitis happens when not enough blood and oxygen flow to the colon tissues and they start to die. Allergic colitis is an allergic reaction in the colon, usually to some food like milk proteins. Finally, microscopic colitis is a chronic condition caused by all sorts of things. It’s called “microscopic” because it can only be diagnosed by microscopic examination of the cells lining the colon.
Does colitis go away?
Colitis symptoms are usually temporary. However, some forms of colitis, particularly ulcerative colitis and microscopic colitis, are chronic conditions. They may oscillate between symptomatic flare-ups and symptom-free remission.
What is the best treatment for colitis?
The best treatment for colitis will depend on the cause. Infectious colitis is often best treated with drugs that eliminate the infection. Ulcerative colitis and microscopic colitis are best treated with drugs that reduce inflammation and prevent flare-ups. Allergic colitis is best treated by taking certain foods out of the diet. Ischemic colitis is an emergency medical situation that usually requires antibiotics, increasing blood flow in the body, and possibly surgery.
What’s next? Additional resources for people with colitis symptoms
Test and diagnostics
Bowel ischemia, StatPearls
Collagenous and lymphocytic colitis, StatPearls
Diagnosis of ulcerative colitis, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
Eosinophilic colitis: epidemiology, clinical features, and current management, Therapeutic Advances in Gastroenterology
Infectious colitis, StatPearls
Treatments
Ulcerative colitis, StatPearls
Ulcerative colitis treatments and medications, SingleCare
Scientific studies and clinical trials
A population-based study of incidence, risk factors, clinical spectrum, and outcomes of ischemic colitis, Clinical Gastroenterology and Hepatology
More information on related health conditions
Crohn’s disease treatments and medications, SingleCare
IBS treatment and medications, SingleCare
What is lactose intolerance? Causes, symptoms, and treatments, SingleCare
Kristi C. Torres, Pharm.D., is a 2005 graduate of The University of Texas at Austin. Her professional background includes academic teaching roles, district-level management for a nationwide pharmacy chain, and clinic-based pharmacy management. Dr. Torres has a wide range of experience in pharmacy operations and has traveled to many states to open and convert clinic-based pharmacies for one of the largest healthcare systems in the nation.
Currently, she works for Tarrytown Expocare Pharmacy in Austin, Texas, serving the intellectual and developmental disability community. There, she leads the order entry team, overseeing orders from across the country.
Dr. Torres began working in pharmacy at the age of 16 in a small East Texas town. She currently resides in Round Rock, Texas, with her daughter and a Shih-Tzu puppy.
...Related Drugs
Related Drug Information
Popular Prescriptions
Support
- Email Us Contact Us
- 24 Hours, 7 Days a Week
(Except Major Holidays)
- Customer Support 844-234-3057
- Provider Support 800-960-6918
Press Center
© 2024 SingleCare Administrators. All Rights Reserved.
* Prescription savings vary by prescription and by pharmacy, and may reach up to 80% off cash price.
Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.
This article is not medical advice. It is intended for general informational purposes and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call your physician or dial 911.
This is a prescription discount plan. This is NOT insurance nor a Medicare prescription drug plan. The range of prescription discounts provided under this discount plan will vary depending on the prescription and pharmacy where the prescription is purchased and can be up to 80% off the cash price. You are fully responsible for paying your prescriptions at the pharmacy at the time of service, but you will be entitled to receive a discount from the pharmacy in accordance with the specific pre-negotiated discounted rate schedule. Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.Towers Administrators LLC (operating as 'SingleCare Administrators') is the authorized prescription discount plan organization with its administrative office located at 4510 Cox Road, Suite 111, Glen Allen, VA 23060. SingleCare Services LLC ('SingleCare') is the vendor of the prescription discount plan, including their website.website at www.singlecare.com. For additional information, including an up-to-date list of pharmacies, or assistance with any problems related to this prescription drug discount plan, please contact customer service toll free at 844-234-3057, 24 hours a day, 7 days a week (except major holidays). By using the SingleCare prescription discount card or app, you agree to the SingleCare Terms and Conditions found at https://www.singlecare.com/terms-and-conditions
© 2024 SingleCare Administrators. All Rights Reserved.