- Home
- Causes Directory
- Vitiligo causes
What causes vitiligo? Diagnosis, prevention, and treatment
Overview: What is vitiligo?
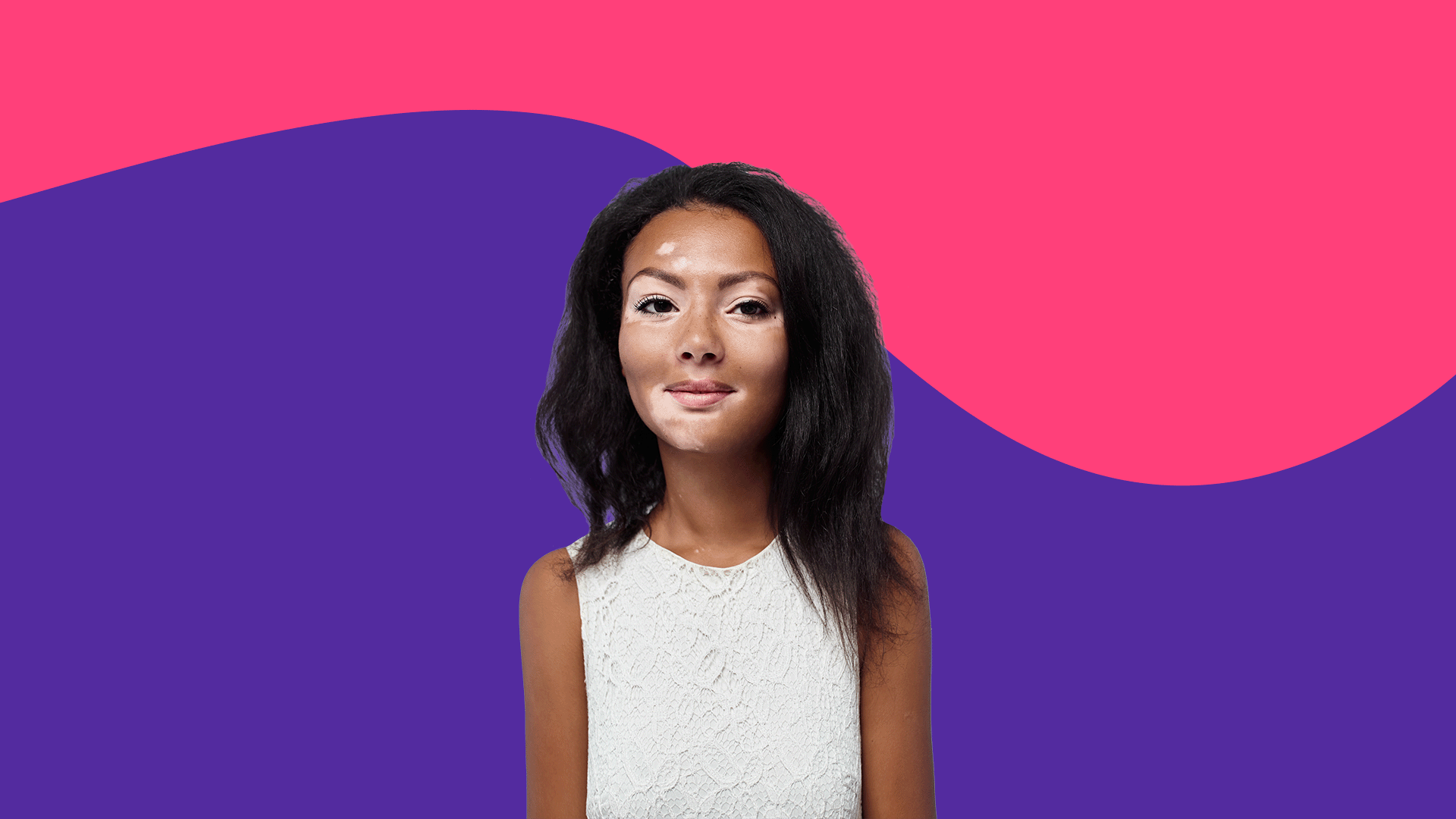
Vitiligo is a chronic autoimmune skin condition in which areas of the skin lose their pigment. This is due to the body’s immune system attacking and destroying the skin cells that produce the skin’s dark pigment (melanocytes). White patches form on the skin. These patches can grow more prominent, or new ones can form elsewhere. The hair in those areas may turn silver or white. These patches can be highly localized, like on the neck or back of the hand. However, the most common type of vitiligo is generalized vitiligo, in which depigmented skin patches appear anywhere on the body. Often, vitiligo appears symmetrical on both sides of the body. Still, it could be a less common segmented subtype where depigmented skin only appears on one side of the body. The eyes and ears can be affected because both have pigment cells. Eye swelling, increased sensitivity to the sun, and even hearing loss are possible. Vitiligo can appear at any age, from child to adulthood but can be more common in teenagers and early adulthood.
Fortunately, vitiligo is not a health-threatening condition, but self-esteem and quality of life can suffer, especially if the affected skin is highly visible.
Key takeaways:
Vitiligo is an uncommon health condition (approximately 0.1% to 2% of people) that can affect anyone regardless of age, sex, race, or ethnicity.
Vitiligo is caused by a complex interaction of genetic and environmental factors that trigger an autoimmune attack on skin pigment cells.
Risk factors for vitiligo include having family members with the condition and having other autoimmune disorders.
Symptoms of vitiligo include loss of pigment on areas of the skin.
Vitiligo usually requires a medical diagnosis.
Vitiligo generally does not require treatment, but medical treatment can help slow the progress of the condition and help restore skin pigment. Vitiligo is a chronic condition, but the effects can be resolved or partly resolved with treatment, though progress is slow.
Vitiligo treatment may include topical drugs that suppress the immune system, phototherapy, and surgery.
Some ways to prevent vitiligo from worsening include avoiding skin damage such as sunburns, tanning beds, cuts, scrapes, and toxic chemicals.
Use coupons for vitiligo treatments, like betamethasone, Protopic (tacrolimus), and Elidel (pimecrolimus), to save up to 80%.
What causes vitiligo?
Healthcare professionals don’t completely understand vitiligo causes. Vitiligo is believed to involve a complex interaction of genetic and environmental factors that trigger an immune system attack on melanocytes. These skin cells produce melanin, the substance that darkens the skin. Without melanocytes to produce melanin, the skin appears pale and white.
Genetic causes of vitiligo: People with vitiligo are born with melanocytes vulnerable to oxidative stress. The release of free radicals, often caused by injury, damages these pigment-producing cells more readily than in other people. People with vitiligo also are born with more active immune system responses to damaged cells, so the immune system is more likely to attack and kill stressed melanocytes.
Environmental causes of vitiligo: The process of vitiligo depigmentation is believed to be triggered by exposure to environmental shock or injuries like severe sunburn, cuts, scrapes, or toxic chemicals.
Though imperfectly understood, vitiligo depigmentation starts when a part of the skin is injured, damaging skin cells. This damage mainly affects melanocytes if they’re genetically vulnerable to free radicals. The stressed melanocytes give off chemicals that attract immune system killer cells. In people genetically susceptible to autoimmune disease, the body’s immune system attacks and destroys melanocytes as if they were foreign invaders. The death of these cells leaves no skin pigment-producing cells in that area. Without melanin, that area of skin and any hair on it may turn white.
Risk factors for vitiligo
Since vitiligo involves a complex interplay between genetics and the environment, the major risk factors for vitiligo are:
A family history of vitiligo
Autoimmune conditions
Exposure to toxic chemicals or skin injuries
Is vitiligo serious? When to see a doctor
Vitiligo is not a life-threatening medical condition but can profoundly affect self-image, self-esteem, mood, and social functioning. People may also develop complications such as eye swelling, increased sensitivity to the sun, and even hearing loss. Certain factors, like the age of vitiligo onset and the amount of body surface involvement, can impact the effectiveness of treatment. Treatment may be more effective if started as early as possible. Still, most people on treatment usually experience periodic cycles of pigment loss and disease stabilization, so visiting a healthcare provider when vitiligo patches first appear is helpful.
How is vitiligo diagnosed?
Vitiligo is diagnosed by examining the skin. At some point, a dermatologist will make the final diagnosis. Dermatologists specialize in skin diseases. The healthcare provider will start by examining the white patches and will also look at those patches with a special ultraviolet lamp called a Wood’s lamp. It’s more popularly known as a black light. It can definitively rule out other causes. In some cases, the healthcare provider may take a skin sample and examine it under the microscope, a procedure called a biopsy. Because vitiligo can affect the eye, an eye doctor may also examine the eye for swelling.
When seeing a dermatologist, be prepared to answer questions like:
When did the problem start?
How have the pigment changes progressed since then?
Have the lesions changed?
What happened before the skin lost pigment?
Are there other symptoms?
Are there any other medical conditions?
What drugs are being taken?
Sometimes a blood test may be needed to discover other possible immune system problems like thyroid disease.
Is vitiligo hereditary?
Vitiligo has a genetic component, though the inheritance is very complex. There is a family history of vitiligo in 25% to 30% of people with vitiligo. People who have a sibling with vitiligo have a 6% chance of developing the same problem. Almost 1 in 4 people with an identical twin with vitiligo also develop the disease. Additionally, many people with vitiligo have other autoimmune diseases, including thyroid disease, Type 1 diabetes, pernicious anemia, rheumatoid arthritis, and psoriasis.
Is vitiligo curable?
Vitiligo is not curable, but it can be treated. The condition’s progress can be slowed down, and repigmentation of blanched areas of skin is possible with drugs, phototherapy, or surgery. Unfortunately, treatment is slow and uncertain. Some people can achieve a complete remission with treatment, but the recurrence rate is high. Treatments are most successful when combination therapy is used.
An effective treatment is UVB light therapy. It works well on early or localized vitiligo. The affected area is bathed in UVB light, which can stimulate the restoration of color to the whitened skin. This treatment option is usually given two to three times a week for six months to one year. UVA light therapy can be used with a drug called psoralen, which makes skin more sensitive to UV light, but this is less common.
Other treatment options include applying topical immunosuppressants to the affected skin, typically corticosteroid or calcineurin inhibitor creams. Topical vitamin D (calcipotriene) or prostaglandin analogues might also be prescribed to restore pigmentation. Some doctors may advise dietary supplements that contain antioxidants to prevent skin cell damage or vitamins and minerals that can help restore pigment. Again, combination treatment is often most effective as it can lead to faster results and greater repigmentation.
For more advanced cases, medications such as oral corticosteroids, systemic immunosuppressants, or the melanocyte-stimulating drug Scenesse (afamelanotide) may be prescribed. Surgical skin grafts or cell transplants can also be used to restore pigment. Skin grafts sound serious, but only small amounts of skin need to be grafted. This healthy skin will provide enough melanin to restore pigment to the entire affected area.
Some people who have lost most of their skin pigmentation may choose to have all the remaining skin pigment removed with a topical medication, such as monobenzone.
How to prevent vitiligo
Although vitiligo is an autoimmune disorder with a genetic component, avoiding environmental triggers can prevent damage to skin pigment cells. The American Academy of Dermatology (AAD) recommends the following measures to prevent vitiligo from spreading:
Avoid sun damage
Always use broad-spectrum, water-resistant SPF 30 or higher sunscreen when exposed to the sun
Apply sunscreen 15 minutes before being exposed to the sun
Wear protective clothing in the sun
Stay in the shade
Do not use tanning beds
Avoid skin injuries like burns, cuts, and scrapes
Protect the areas of the body most vulnerable to scrapes and cuts, such as hands, elbows, and knees
Most importantly, see a dermatologist as early as possible
Vitiligo is not curable, but treatment can slow its progress and restore skin pigment to affected areas. Treatment may be most successful when started early, so talk to a healthcare professional when the first symptoms appear.
FAQs about vitiligo causes
What causes vitiligo to spread?
Vitiligo can be triggered by skin injuries such as sunburns or scrapes, so dermatologists advise people with vitiligo to protect their skin from injuries and the sun. Emotional and physical stress might also contribute to the spread of vitiligo. Stress increases immune system activity and is associated with the worsening of other autoimmune diseases, such as inflammatory bowel disease (IBD) and rheumatoid arthritis.
What causes vitiligo to get worse?
Anything that causes skin damage or triggers the immune system can worsen vitiligo. This includes cuts, scrapes, burns, emotional stress, and physical stress.
Is vitiligo related to liver disease?
Vitiligo is an autoimmune disease, but the genetics are complicated. Nonetheless, people with vitiligo have an increased risk of developing other autoimmune diseases, particularly thyroid disease, Addison’s disease (an autoimmune disease of the adrenal glands), and Type 1 diabetes (an autoimmune disease of the pancreas). There is also an association between vitiligo and autoimmune disorders of the liver, such as autoimmune hepatitis.
What’s next? Additional resources for people with vitiligo
Test and diagnostics
Vitiligo, StatPearls
Treatments
Recent advances in understanding vitiligo, F1000Research
Surgical interventions for patients with vitiligo: a systematic review and meta-analysis, JAMA
Vitiligo: a narrative review, Cureus
Vitiligo: diagnosis and treatment, American Academy of Dermatology (AAD)
Vitiligo: diagnosis, treatments, and steps to take, National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Scientific studies and clinical trials
Skin manifestations associated with autoimmune liver diseases: a systematic review, Clinical Reviews in Allergies & Immunology
Vitiligo pathogenesis and emerging treatments, Dermatologic Clinics
More information on related health conditions
Stephanie Melby, B.S., Pharm.D., received a bachelor of science in nutrition from the University of Minnesota and a doctorate of pharmacy from the University of New England. She has seven years of experience in retail pharmacy and is certified in Medication Therapy Management (MTM). Dr. Melby resides in Minneapolis, Minnesota.
...Related Drugs
Related Drug Information
Popular Prescriptions
Support
- Email Us Contact Us
- 24 Hours, 7 Days a Week
(Except Major Holidays)
- Customer Support 844-234-3057
- Provider Support 800-960-6918
Press Center
© 2024 SingleCare Administrators. All Rights Reserved.
* Prescription savings vary by prescription and by pharmacy, and may reach up to 80% off cash price.
Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.
This article is not medical advice. It is intended for general informational purposes and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call your physician or dial 911.
This is a prescription discount plan. This is NOT insurance nor a Medicare prescription drug plan. The range of prescription discounts provided under this discount plan will vary depending on the prescription and pharmacy where the prescription is purchased and can be up to 80% off the cash price. You are fully responsible for paying your prescriptions at the pharmacy at the time of service, but you will be entitled to receive a discount from the pharmacy in accordance with the specific pre-negotiated discounted rate schedule. Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.Towers Administrators LLC (operating as 'SingleCare Administrators') is the authorized prescription discount plan organization with its administrative office located at 4510 Cox Road, Suite 111, Glen Allen, VA 23060. SingleCare Services LLC ('SingleCare') is the vendor of the prescription discount plan, including their website.website at www.singlecare.com. For additional information, including an up-to-date list of pharmacies, or assistance with any problems related to this prescription drug discount plan, please contact customer service toll free at 844-234-3057, 24 hours a day, 7 days a week (except major holidays). By using the SingleCare prescription discount card or app, you agree to the SingleCare Terms and Conditions found at https://www.singlecare.com/terms-and-conditions
© 2024 SingleCare Administrators. All Rights Reserved.