- Home
- Symptoms Directory
- Rheumatoid arthritis symptoms
Rheumatoid arthritis symptoms: What are the early signs of rheumatoid arthritis?

Overview: What does rheumatoid arthritis feel like?
Rheumatoid arthritis (RA) is an autoimmune disease in which the immune system attacks the tissues in the joints. As rheumatoid arthritis progresses, it can also cause problems in other organs. The first joints that are affected tend to be smaller ones, like those in the fingers and toes, but as the disease progresses, other joints are involved.
Rheumatoid arthritis is painful and disabling. Joint pain, stiffness, and swelling are all initial symptoms. As more fingers are affected, people lose strength in their grip and the ability to use their hands. As larger joints become involved, they lose their range of motion. Walking, lifting, and other tasks become difficult.
Rheumatoid arthritis is a progressive and chronic disease that can cause severe disability, other illnesses, and premature death if untreated or if treatment fails. However, when it is caught and treated early, the prognosis can be more positive.
Key takeaways:
Rheumatoid arthritis affects over 1.3 million people in the United States and can affect anyone regardless of age, sex, race, or ethnicity—although it is more common in women than men, and more likely to develop between ages 30 to 60 years of age.
Early signs of rheumatoid arthritis include pain, stiffness, and swelling in finger and toe joints. Fatigue, muscle pain, mood changes, and low-grade fever may also occur.
Serious symptoms of rheumatoid arthritis or its complications such as infections, lung problems, chest pain, and shortness of breath, may require immediate medical attention.
Rheumatoid arthritis may be caused by a combination of genetic and environmental factors. You may be at higher risk for developing rheumatoid arthritis symptoms if you have a relative with rheumatoid arthritis, if you are a woman, if you’re older, if you smoke, have had gingivitis, or if you are exposed to environmental toxins such as asbestos, silica, or textile dust.
Rheumatoid arthritis requires a medical diagnosis.
Symptoms of rheumatoid arthritis generally do require treatment. They may resolve or partially resolve with treatment, but it will vary from person to person. If treatment is started within three months after the appearance of symptoms, there is a better chance of sustained remission.
Treatment of rheumatoid arthritis may include antirheumatic drugs, corticosteroids, pain relievers, physical therapy, and occupational therapy. Some individiauls may need surgery. Read more about rheumatoid arthritis treatments here.
Untreated rheumatoid arthritis could result in complications like severe disability, skin disorders, anemia, lung disease, cancer, serious infections, bone loss, blood clots, heart problems, coronary artery disease, and premature death.
Save on prescriptions for rheumatoid arthritis with a SingleCare prescription discount card.
What are the early signs of rheumatoid arthritis?
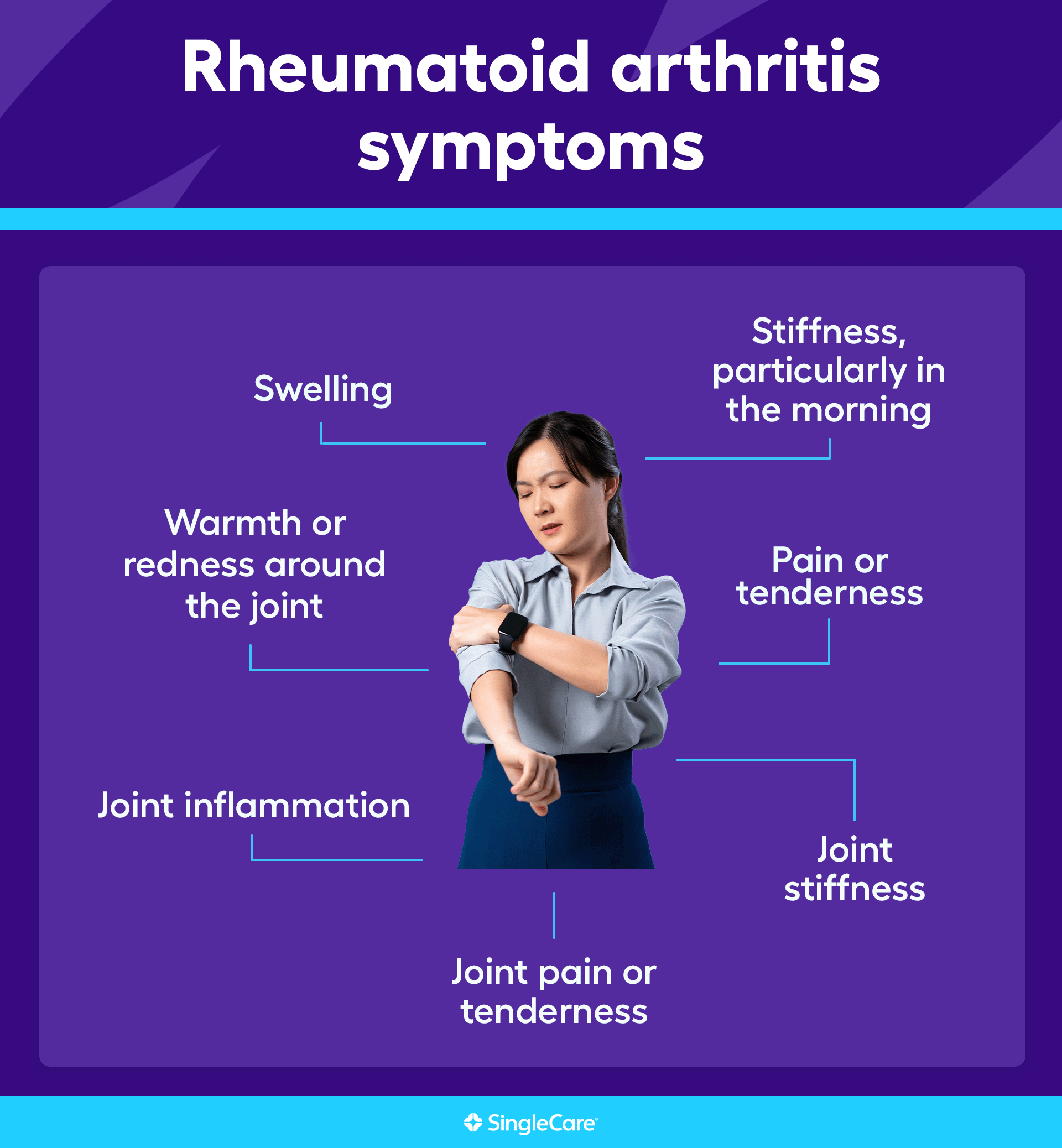
The earliest warning signs of rheumatoid arthritis typically involve the small joints in the fingers and toes, but it could start in larger joints like the ankles or knees. These early joint symptoms include:
Swelling
Pain or tenderness
Stiffness, particularly in the morning
Warmth or redness around the joint
The swelling, called synovitis, can feel spongy because of fluid build-up.
Other rheumatoid arthritis symptoms
The joint symptoms associated with rheumatoid arthritis include:
Joint inflammation
Joint pain or tenderness
Joint stiffness
Warmth or redness around the joint
These can be present in small joints or large joints. In rheumatoid arthritis, joints are most commonly affected on both sides of the body.
Other symptoms of rheumatoid arthritis include:
Fatigue
Weight loss
Low-grade fever
As RA advances, other symptoms may include:
Involvement with multiple joints
Joint deformity
Reduced grip strength
Reduced range of motion of the affected joints
Joint immobility
Disability and problems with occupational or daily activities
Rheumatoid nodules (firm bumps around or near the affected joints)
Symptoms of other disorders such as blood vessel swelling, lung diseases, anemia, infections, cancer, or coronary artery disease (CAD)
Rheumatoid arthritis vs. osteoarthritis symptoms
Rheumatoid arthritis is an autoimmune inflammatory arthritis in which the immune system causes swelling and damage in the joints. The inflammatory response damages tissues in the affected joints and can cause bone loss. On the other hand, osteoarthritis is due to a breakdown of joint cartilage between bones. These changes can be caused by injury, age, wear and tear, or other factors, but the cartilage in one or more joints loses the ability to properly repair and restore itself. As a result, the cartilage wears down, and the bones start rubbing against each other, causing swollen and painful joints. The most important difference between rheumatoid arthritis and osteoarthritis is that osteoarthritis is limited to the affected joints while rheumatoid arthritis is an inflammatory disease that can affect multiple organs, including the skin, eyes, lungs, blood vessels, and heart.
| Rheumatoid arthritis | Osteoarthritis | |
| Shared symptoms |
|
|
| Unique symptoms |
|
|
RELATED: Osteoarthritis vs. rheumatoid arthritis: which one do I have?
Stages of rheumatoid arthritis: How can I tell which one I have?
Rheumatoid arthritis is a progressive condition in which joint damage steadily worsens. These stages of joint damage are as follows:
Stage I: There may be mild symptoms of rheumatoid arthritis such as joint pain and stiffness
Stage II: Inflammation continues, causing worsening of symptoms. Joint and bone damage may begin.
Stage III: The bones begin to fuse together with connective tissue, which limits range of motion. Affected joints may appear crooked and bent.
Stage IV: Bones fuse together with bone tissue. Pain may subside, but movement and daily activities are severely limited.
It can take many years to go through the stages, and not all individuals with rheumatoid arthritis will go through all stages. Some individuals will have periods of time without rheumatoid arthritis activity, called remission. .
When to see a doctor for rheumatoid arthritis symptoms
If joint problems are due to rheumatoid arthritis, the prognosis is determined by how early a diagnosis is made and treatment is started. This is also true of osteoarthritis since it is always diagnosed after the joint is irreversibly damaged. Always see a doctor if you have any symptoms of arthritis: joint pain, joint swelling, stiffness, and joint tenderness.
Diagnosing rheumatoid arthritis is challenging. The doctor will perform a physical examination and take a detailed medical history. To diagnose RA, the doctor will use a scale (called the Rheumatoid Arthritis Severity Scale) and base the diagnosis on:
The symptoms and the number of joints that are affected
Blood tests that identify definitive markers of rheumatoid arthritis such as rheumatoid factor or certain antibodies called ACPA
The doctor will also test the blood for identifying markers of active inflammation including the speed at which red blood cells fall to the bottom of a test tube (erythrocyte sedimentation rate or ESR) and the amount of a protein (C-reactive protein or CRP) that is involved in inflammatory responses.
In some cases, the doctor may test the joint fluid to rule out other problems such as infection.
RELATED: What are normal CRP levels?
Complications of rheumatoid arthritis
Treatment does not always work, so complications of rheumatoid arthritis can happen to both treated and untreated patients, though untreated patients are at an increased risk of complications. As an inflammatory disease, rheumatoid arthritis affects other parts of the body, so the complications of rheumatoid arthritis include:
Blood vessel swelling
Eye disorders and eye pain
Buildup of a protein (amyloid) in the body’s organs (amyloidosis)
Nerve damage
Fluid buildup around the lungs
Interstitial lung disease
Serious infections
Bone loss
Blood clots
Hardening of the arteries
Heart disease, including coronary artery disease
Certain types of cancer
Premature death
How to treat rheumatoid arthritis symptoms
Rheumatoid arthritis does require treatment to avoid complications and increase the quality of life. Most people will be treated by a physician, and a specialist in rheumatic disorders called a rheumatologist.
The primary treatments for rheumatoid arthritis are called “disease-modifying antirheumatic drugs” or DMARDs. These are either biologic drugs (drugs made from biological sources such as monoclonal antibodies) or nonbiologic drugs like methotrexate. Both suppress or control the immune system to prevent inflammation and joint damage. They are used both during an attack and as a maintenance treatment to prevent flare-ups. An active bout with RA or joint pain may be treated with corticosteroids to reduce inflammation and nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and swelling.
Important complementary treatments include physical therapy and occupational therapy to help people improve muscle strength and daily functioning. Some natural treatments and Tai Chi have been shown to have some benefits, too.
RELATED: What is methotrexate? Uses, warnings, & interactions
Living with rheumatoid arthritis
Rheumatoid arthritis is a chronic disease. The primary goals of living with rheumatoid arthritis are to prevent relapses, slow the progress of the disease, and live the best possible life. To do that:
Take the prescribed drugs as instructed.
Keep all appointments with healthcare providers, doctors, and the rheumatologist
Do the exercises prescribed in physical therapy and occupational therapy
Follow any dietary guidelines
Keep a side effects and symptom diary to share with healthcare professionals at each appointment
Practice Tai Chi or yoga to help develop strength or range of motion
Quit smoking
Eat a healthy diet
Get plenty of sleep
Participate in a support group
Start making plans for financial support if the condition worsens
RELATED: Living with a condition that strangers think you’re ‘too young’ to experience
Most importantly, see a doctor as soon as possible
When symptoms appear, don’t hesitate to see a doctor. Early treatment can prevent permanent joint damage or worsening of the condition. No type of arthritis can be self-diagnosed or self-treated. A doctor or specialist is required. Treatment will vary depending on the type of arthritis.
FAQs about rheumatoid arthritis symptoms
What are the first signs of rheumatoid arthritis?
The typical first signs of rheumatoid arthritis are pain, tenderness, swelling, warmth, and stiffness in one or more small joints. In some cases, a large joint like the knee or ankle could be involved. During an active flare-up, symptoms like fatigue and a low fever may be experienced, as well.
What does rheumatoid pain feel like?
Rheumatoid pain can vary. Many people experience aching, throbbing, burning, or intense pain in the joints. But the inflammatory process associated with rheumatoid arthritis can affect the rest of the body, so general aches and fatigue are possible, as well.
What triggers your rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune inflammatory condition that may have a genetic component and can be triggered by environmental factors. The most common environmental trigger is cigarette smoking, but other possible culprits include asbestos, textile fibers, silica, and gingivitis (bacterial gum infection). The trigger gets the immune process going, it doesn’t cause symptoms of RA. After being triggered, it can take several years before symptoms appear. During all this time, the body produces antibodies that will eventually target the joints, so it is possible to identify someone with rheumatic disease before any symptoms occur.
What’s next? Additional resources for people with rheumatoid arthritis symptoms
Test and diagnostics
Diagnosis and management of rheumatoid arthritis, American Family Physician
Rheumatoid arthritis, StatPearls
Rheumatoid arthritis: common questions about diagnosis and management, American Family Physician
Treatments
Diagnosis and management of rheumatoid arthritis, American Family Physician
Rheumatoid arthritis, StatPearls
Tips for living with RA, Arthritis Foundation
Scientific studies and clinical trials
Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis, Cochrane Database of Systematic Reviews
Rheumatoid arthritis: early diagnosis and treatment options, Caspian Journal of Internal Medicine
More information on related health conditions
Arthritis treatments and medications, SingleCare
Gout treatment and medications, SingleCare
Osteoarthritis vs. rheumatoid arthritis: which one do I have?, SingleCare
Psoriasis treatments and medications, SingleCare
After receiving her doctorate from the University of Pittsburgh School of Pharmacy, Karen Berger, Pharm.D., has worked in both chain and independent community pharmacies. She currently works at an independent pharmacy in New Jersey. Dr. Berger enjoys helping patients understand medical conditions and medications—both in person as a pharmacist, and online as a medical writer and reviewer.
...Related Drugs
Related Drug Information
Popular Prescriptions
Support
- Email Us Contact Us
- 24 Hours, 7 Days a Week
(Except Major Holidays)
- Customer Support 844-234-3057
- Provider Support 800-960-6918
Press Center
© 2024 SingleCare Administrators. All Rights Reserved.
* Prescription savings vary by prescription and by pharmacy, and may reach up to 80% off cash price.
Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.
This article is not medical advice. It is intended for general informational purposes and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, immediately call your physician or dial 911.
This is a prescription discount plan. This is NOT insurance nor a Medicare prescription drug plan. The range of prescription discounts provided under this discount plan will vary depending on the prescription and pharmacy where the prescription is purchased and can be up to 80% off the cash price. You are fully responsible for paying your prescriptions at the pharmacy at the time of service, but you will be entitled to receive a discount from the pharmacy in accordance with the specific pre-negotiated discounted rate schedule. Pharmacy names, logos, brands, and other trademarks are the property of their respective owners.Towers Administrators LLC (operating as 'SingleCare Administrators') is the authorized prescription discount plan organization with its administrative office located at 4510 Cox Road, Suite 111, Glen Allen, VA 23060. SingleCare Services LLC ('SingleCare') is the vendor of the prescription discount plan, including their website.website at www.singlecare.com. For additional information, including an up-to-date list of pharmacies, or assistance with any problems related to this prescription drug discount plan, please contact customer service toll free at 844-234-3057, 24 hours a day, 7 days a week (except major holidays). By using the SingleCare prescription discount card or app, you agree to the SingleCare Terms and Conditions found at https://www.singlecare.com/terms-and-conditions
© 2024 SingleCare Administrators. All Rights Reserved.