When blood appears in a bowel movement, that’s because some part of the digestive tract is bleeding. The bleeding can be anywhere, but if bright red blood is in the poop, that usually means the small intestine, large intestine, or rectum is bleeding. If the bleeding is in the upper GI tract, it usually doesn’t look like blood. Instead, it’s dark and tarry. No matter what the source, the blood may appear once and then go away. However, blood in the stools can keep coming back. Bowel movements are fine for a while, and then blood shows up again. Sometimes, blood in the poop never lets up.
That’s what it looks like. What does it feel like? In some cases, it feels like nothing. In many other cases, blood in the stools will be accompanied by other symptoms, usually pain. It can range from mildly discomforting to excruciating. There may be other symptoms such as diarrhea or weight loss depending on the cause. However, the symptoms to worry about are those related to blood loss. Symptoms like a fast heart rate, feeling faint when standing, and low blood pressure may indicate that the body is losing too much blood. That’s when emergency treatment is needed.
Bleeding causes blood in the stools. That’s the simple answer. The question is, from where and why? The digestive tract is so large (30 feet long, about two stories) and so complex, that the possible causes are unmanageably numerous.
Since lower gastrointestinal bleeding shows up as bright red blood and upper gastrointestinal bleeding appears dark maroon, black, and tarry, that’s a good way to divide up the possible causes of blood in the stool.
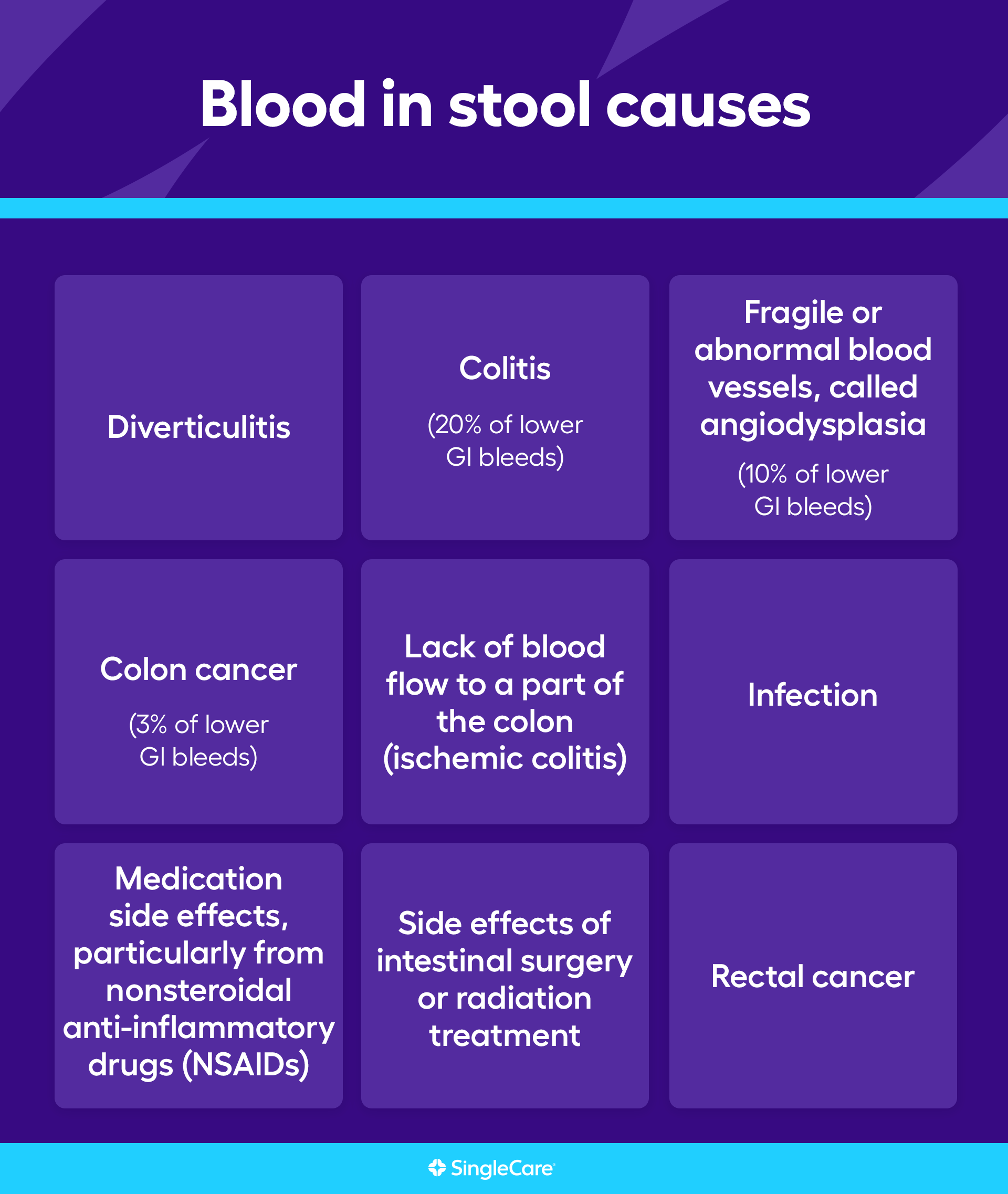
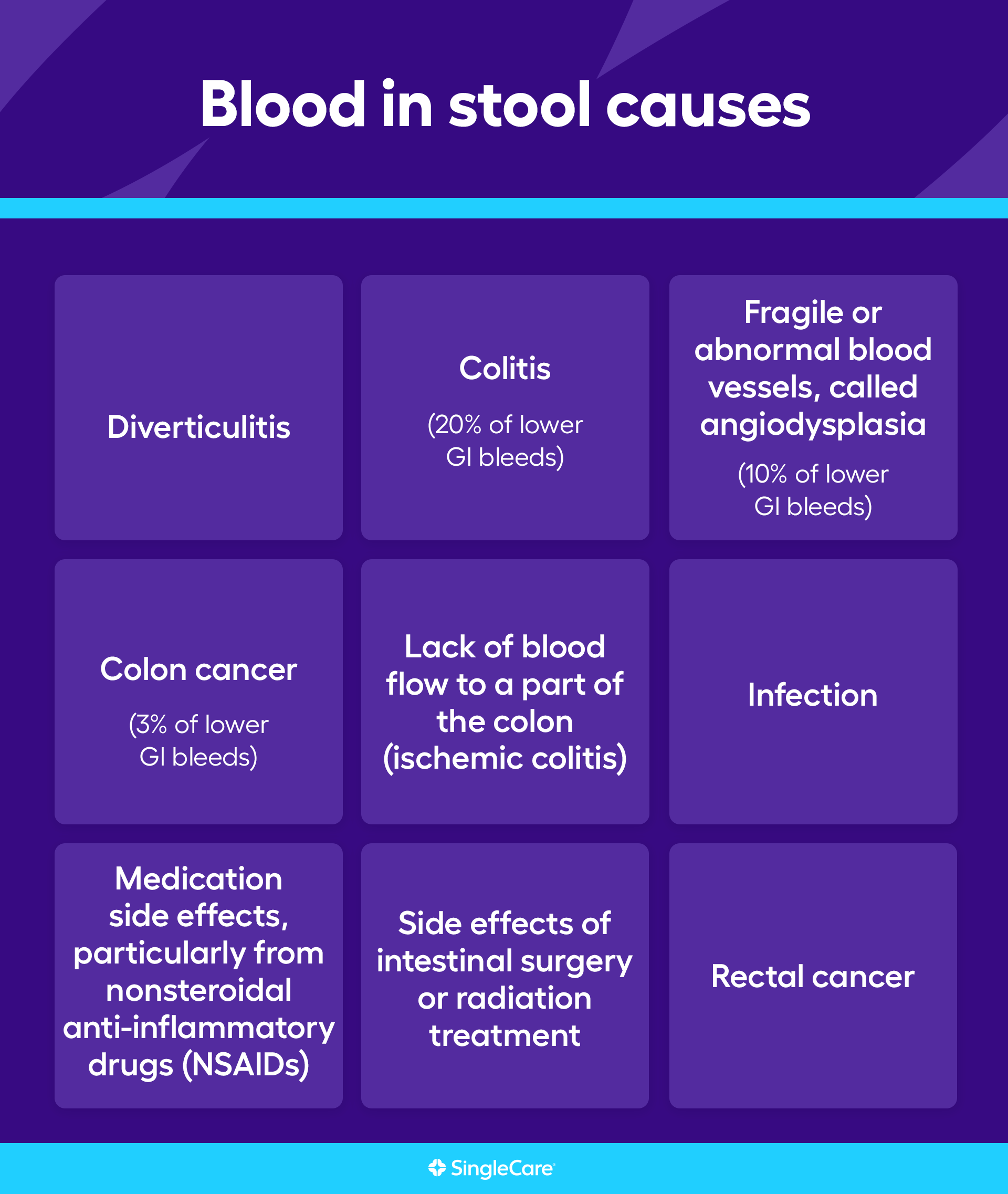
Diverticulitis is the most common cause of lower gastrointestinal tract bleeding, accounting for about 30% to 40% of cases. Diverticulitis is a complication of diverticulosis, a condition in which pouches (diverticula) balloon out of the bowel. When these become swollen, they can bleed into the colon.
Other common causes of lower GI tract bleeding include:
Colitis (20% of lower GI bleeds)
Fragile blood vessels (10% of lower GI bleeds)
Crohn’s disease
Ulcerative colitis
Abnormal blood vessels (angiodysplasia)
Colon cancer (3% of lower GI bleeds)
Infection
Artery rupture
Colorectal polyps (growths in the colon)
Medication side effects, particularly from nonsteroidal anti-inflammatory drugs (NSAIDs)
Side effects of intestinal surgery or radiation treatment
Lower GI tract bleeding can be caused by rectal and anal problems including:
The most common causes of upper GI tract bleeding are:
Peptic ulcer disease (40% to 50% of cases)
Duodenal ulcers (30%)
Erosive esophagitis
Swelling of the duodenum
Blood vessel problems (varices)
Esophageal tears
Perforated artery
Cancer
Foreign objects
Surgery
Medication side effects, particularly NSAIDs
While most of these conditions produce black and tarry stools, a massive upper GI tract bleed could show up as red blood in the stools. A massive bleed anywhere in the digestive system will quickly produce symptoms of significant blood loss.
Keep in mind that bloody stool isn’t always due to digestive diseases. It may be due to mundane causes such as overusing toilet paper or passing hard stools which can cut small tears on the rectum.
RELATED: What does a diverticulitis attack feel like?
Blood in the stools could be a sign of a serious condition. If it doesn’t stop, then the bleeding itself needs medical attention.
Here's the problem: when blood appears in the stools, something’s bleeding. What’s bleeding and why can’t be visually determined like bleeding from a skin wound can be. Without the help of a healthcare professional, there’s little way to figure out if blood in the stool is something to worry about or nothing to worry about.
Most of the time, blood in the stool is nothing to worry about. In 80% of the cases when blood appears in the stool, it will resolve spontaneously and never come back. However, even if resolves quickly and doesn’t come back, there may be a gastrointestinal problem more serious than just bleeding, like cancer. Tell a healthcare professional about the incident.
If the bleeding keeps coming back or never stops, then there’s no question that medical help is needed.
Emergency medical help is needed if there is a lot of blood in the stool or there are any signs of blood loss such as fast heartbeats, low blood pressure, or feeling faint when standing up.
RELATED: Colon cancer symptoms: what are the early signs of colon cancer?
Diagnosing blood in the stool can be tricky. There are many possible causes and many symptoms to sift through. However, before anything else is investigated, the healthcare provider will try to determine if blood loss is a problem. This will usually involve taking vital signs such as checking the heart rate and measuring blood pressure. If blood loss is a problem, then that needs to be treated immediately with restorative treatments.
If blood loss is not a problem, then the healthcare professional will try to identify both the location and cause of the bleeding. This will take more work. Symptoms are important, so be prepared to answer questions about when the blood appeared, how quickly the incident resolved, and any accompanying symptoms. Previous medical conditions can also help determine the cause, so be prepared to tell the clinician about previous medical problems, surgeries, medications, supplements, and if there’s any family history of blood in the stools.
A physical exam will provide more clues. The clinician may palpate the abdomen to find tender spots or feel for masses. A rectal examination will usually be conducted. Of course, stool tests may be needed. Blood tests can also help spot causes like infections or inflammatory issues.
Unless the answer is pretty obvious, like hemorrhoids, chances are a gastroenterologist will be called in to do more diagnostics. Gastroenterologists are doctors that specialize in diseases of the digestive system. If upper GI tract bleeding is suspected, the gastroenterologist will inspect the esophagus, stomach, or duodenum with a camera attached to a long thin tube, a procedure called an endoscopy. The doctor will use a similar device to examine the colon if a lower GI tract problem is suspected, only the procedure is called a sigmoidoscopy or colonoscopy. This may require an extra day to clear all the contents out of the colon.
If the doctor suspects active bleeding and endoscopy does not reveal the source, a CT scan or imaging using a contrast dye will be required.
Blood in the stool is not contagious. However, if it’s caused by an infection, that infection is contagious. Gastrointestinal infections are usually marked by symptoms such as diarrhea, watery diarrhea, change of bowel habits, and abdominal pain or tenderness. Fever is another common symptom. Bloody diarrhea is a symptom of some intestinal infections. Gastrointestinal infections can be prevented with good hygiene and safe food preparation.
Blood in the stool lasts for as long as the bleeding lasts. That’s usually not long. 80% of lower gastrointestinal bleeding and 95% of rectal bleeding goes away spontaneously. Continuous bleeding or repeated bleeding may not go away until the wound is closed or the underlying condition is treated. Heavy bleeding requires emergency medical treatment to stop the bleeding.
If blood in the stool is not a one-time, short-duration problem, then medical treatment is probably needed. If the bleeding is excessive, then emergency treatment may be needed.
In some cases of recurrent bleeding episodes such as hemorrhoids or ulcers, people may be sent home with prescription medications such as proton pump inhibitors (for ulcers), antibiotics (for infections), or over-the-counter medications such as vasoconstrictors (for hemorrhoids). In other cases, the bleeding may be easy to identify and then corrected with in-office medical procedures. More serious cases may require more involved surgery.
Nonstop bleeding or notable blood loss will be treated in an emergency room or intensive care unit. The immediate crisis is to restore blood volume through IV fluids and to stop the bleeding using blood clotting medications. In cases of severe blood loss, a blood transfusion may be needed. In severe bleeding cases, the bleeding will be stopped using surgical procedures.
Stress does not cause blood in the stool. However, it can exacerbate conditions such as Crohn’s disease or ulcerative colitis.
Foods do not cause blood in the stools. However, some foods may turn stools red, possibly giving people a bit of a scare. Red food coloring is a common culprit and it’s usually found in processed foods like red licorice. Beets, cranberries, Tandoori powder, and other bright red foods can color poop red, even bright red. Likewise, black foods can make stools appear black. Again, the most common culprit is dark food dye.
Dehydration does not cause blood in the stool, but it can cause hard and difficult-to-pass stools. Passing hard stools may scratch or tear the rectum which will then bleed for a bit.